If "masks work", why don't they work? New research suggests the reason.
A recently released study investigating the efficacy of masks at filtering aerosols in the 0.2 - 1 micron range, suggests answers to the disconnect between the results of mechanistic studies and RCTs.
It may seem that the mask wars are over, and a question like this is re-litigating the past, drawing us back into the fraught days of COVID. And yet, as one of the most contentious policies of that period, and something which in healthcare settings is in many places becoming established as a norm, it remains an important question. It is an especially important question if we truly want to provide real protection from disease to healthcare workers and immunocompromised people, not just iron-clad legal protection for providers and employers.

A newly published scientific study from the University of Waterloo, makes an effort to understand the disconnect between the demonstrated mask efficacy in mechanistic and observational studies, and the uncomfortable reality that, in the words of the paper’s authors, “population-wide adoption of masking has not provided a concordant curbing of disease spread (Centers for Disease Control and Prevention 2021; Schauer et al. 2021).” (See also CDC, 2020, and Jefferson et al, 2023. for systemic reviews.)
As the CDC noted in its review of masks and other interventions in May of 2020 “Although mechanistic studies support the potential effect of hand hygiene or face masks, evidence from 14 randomized controlled trials of these measures did not support a substantial effect on transmission of laboratory-confirmed influenza. (. . . ) We identified several major knowledge gaps requiring further research, most fundamentally an improved characterization of the modes of person-to-person transmission.” (Emphasis added).
The important thing this study does is to take into account what we have learned about these different modes of transmission of respiratory viruses since the beginning of COVID. Armed with that knowledge, it embarks on a mechanistic study with different experimental protocols than prior studies. These protocols better reflect our current understanding of person-to-person transmission. If these protocols do, in fact, better reflect the mechanism of transmission, the results of this study should help to answer the question, “If masks work [in some studies], why don’t they work [in real life]?” The exciting thing? It does just that.
Let’s first dissect the disconnect. Mechanistic studies don’t directly evaluate the thing with which you are concerned, in this case, the ability of mask-wearing to stop someone from passing a respiratory disease to another person. Mechanistic studies try to simulate the situation and evaluate it using that mechanism (this is cheaper and safer than using actual sick people). In the case of mask studies, mechanistic studies are generally done with mannequins that have a simulated breathing apparatus.
The problem with mechanistic studies is, if you get the mechanism wrong, the results will mislead you. And that is exactly what appears to have happened with prior mechanistic studies. This is precisely why the CDC noted in the above excerpt that “we need to better understand the modes of person-to-person transmission, in order to design studies that better reflect the reality of how respiratory diseases spread.” Based on the discordant results between some kinds of lower quality evidence (mechanistic and observational studies) and other kinds of higher quality evidence (randomized controlled trials, and systemic reviews of such), logic argues that the mechanism of transmission used to simulate transmission in the mechanistic studies is likely wrong. This would explain the different results between the mechanistic studies that show such promise, and the higher-evidence-quality randomized controlled trials (RCTs) that show very different results.
All will recall early in the COVID years, an obsession with keeping surfaces clean in order to avoid contracting COVID via “fomites.” Gradually it became clear that this type of transmission was not a major driver of infections, and that COVID was airborne, spread largely via aerosols. This is when mechanistic mask studies really took off. You’ll recall early on, doctors were ventilating patients to avoid “aerosol-generating procedures”, but the aerosols they were concerned with stopping were those generated from coughing and other larger aerosols, generally in the 5-100 micron size.
Indeed, to this day, the CDC still (ahem…Trump administration…) has this mode of transmission up on its website as the primary mode of viral respiratory infections.
Excerpt 1

The good news about this potential mode of transmission—and I believe one of the reasons the public health community have been so unwilling to reconsider it—is that these larger aerosols are easily captured with just a simple surgical, or even cloth, mask. From Milton et al, 2013:
Excerpt 2
Unfortunately, while that study shows mask efficacy at containg aerosols over 5 microns, the same study shows that the vast majority of virus are not found in aerosols of this size, but rather in the fine aerosols—those under 5 microns, and those which the study notes are not well-contained by masks (see highlight, in Excerpt 3 below).
Excerpt 3

Worse still, the authors found infectious virus only among the fine aerosols, those less than 5 microns. Further, these fine aerosols had nearly 9 times the number of viral copies than the coarse particles. This means that while the masks were effective at stopping the dissemination of the coarse aerosols over 5 microns, that capture was functionally meaningless, because the aerosols captured a) contained nearly 10x less virus than the fine aerosols, and b) at least in this study, the virus the masks did capture was not capable of causing infections.
Excerpt 4
This finding—that the vast majority of virus, and to date, virtually the only infectious virus, is found in the fine aerosols—continues to be duplicated. It has now been found in a 2013 study, when 89% of infectious virus was found in fine aerosols (<5 microns), and a 2022 study that only found infectious virus in the fine aerosols that had escaped from a mask-wearing participant. Further, when investigated more granularly in the <5 micron range, infectious aerosols were only found in the 0.25 - 0.5 micron range.
Indeed, based on pre-2020 research, and some 2020 research, a July 2020 study pointed out that breathing is enough when it comes to the ability to spread COVID. This study noted that, based on a large volume of research from as early as 1997, the vast majority of aerosols generated during any mode of exhalation, whether breathing, coughing, or otherwise, are less than one micron, with the median around 0.28 microns, and “Only a small droplet fraction of about 2% was located in the super micron [i.e. larger than 1 micron] range, with no particles larger than 5 microns” (see excerpt 5 below). Further, the authors also cited various works noting that infectious virus has repeatedly been found predominantly in the most numerous aerosols—those under 1 micron.
Excerpt 5

Despite a rather robust catalogue of research prior to 2020 suggesting a significant, if not overwhelming role for sub-micron aerosols in disease transmission, the vast majority of mask studies have focused predominantly on stopping those aerosols over 5 microns. Until this new paper, virtually none of these studies looked at aerosols less than 1 micron, much less in the 0.25 - 0.5 micron range where infectious virus is most often found, and which represent by far the lion’s share of the aerosols that we exhale. This is why this paper is a very important paper. Let’s dig in.
As noted previously, the experimental set-up in this study varies from other mechanistic mask studies. There were two parts to this study. The first attempted to identify and quantify various mask types’ effectiveness in filtering aerosols < 1 micron. The second evaluated the flow of particles from each mask type.
Like other studies before it, this study fitted various masks (surgical, KN95, and N95) to a mannequin in a closed chamber, adhering to the manufacturers’ guidelines for fitting (pinching the nose, minimizing gaps). What was different about this set-up, is that the aerosols that were generated better mimicked the physiological distribution of aerosols exhaled by humans—being in a size range of 0.2 microns - 1 micron—with the average at 0.5 micron (still larger than the average of those exhaled by humans in “real life”, which is 0.28 microns). The breathing apparatus mimicked the breathing of an adult male, breathing at a rate of ~14 breaths/minutes, with each breath exhaling ~586 mL. The chamber was a small closed chamber (0.64 m x 0.64 m x 0.91 m), and the breathing apparatus was run for 30 minutes past when a “steady state” was achieved (more on this in the last section)—approximately 1.5 hours. They also did tests to test the mask filtration in the absence of any gaps, using the same breathing apparatus and parameters, but attaching a mask holder to the mannequin with the mask secured over the outlet with rubber gaskets. This was important in order to demonstrate that the masks being evaluated demonstrated the same filtration efficiency as those in other studies.
The results are below. I’ll walk through the highlights after the tables.
Excerpt 6 below shows surgical masks having an average filtration efficiency of ~20%, with error bars dropping down to virtually 0% KN95s at ~40%, and dropping down well into the range of surgical masks, and N95s at ~62%, getting close to 80% at the top end. This is all markedly lower than their material filtration efficiencies, which are shown in the lower plot below, figure 7(b).
Excerpt 6

This is, however, not unexpected. Excerpt 7 shows the results of a study done in early 2020 showing filtration efficiencies for different types of masks with gaps of 1%, and without. Based on this, it seems that the high-end range of the error bars in the plot above likely correspond to the times when the researchers were able to keep the gap closer to 1%, and the lower end when those gaps were larger. Extrapolation from a study by Drewnick et al, suggests that just a 3.2% gap would be sufficient to render a surgical mask 0% effective—the data presented in excerpt 6 above would seem to corroborate that.
Excerpt 7

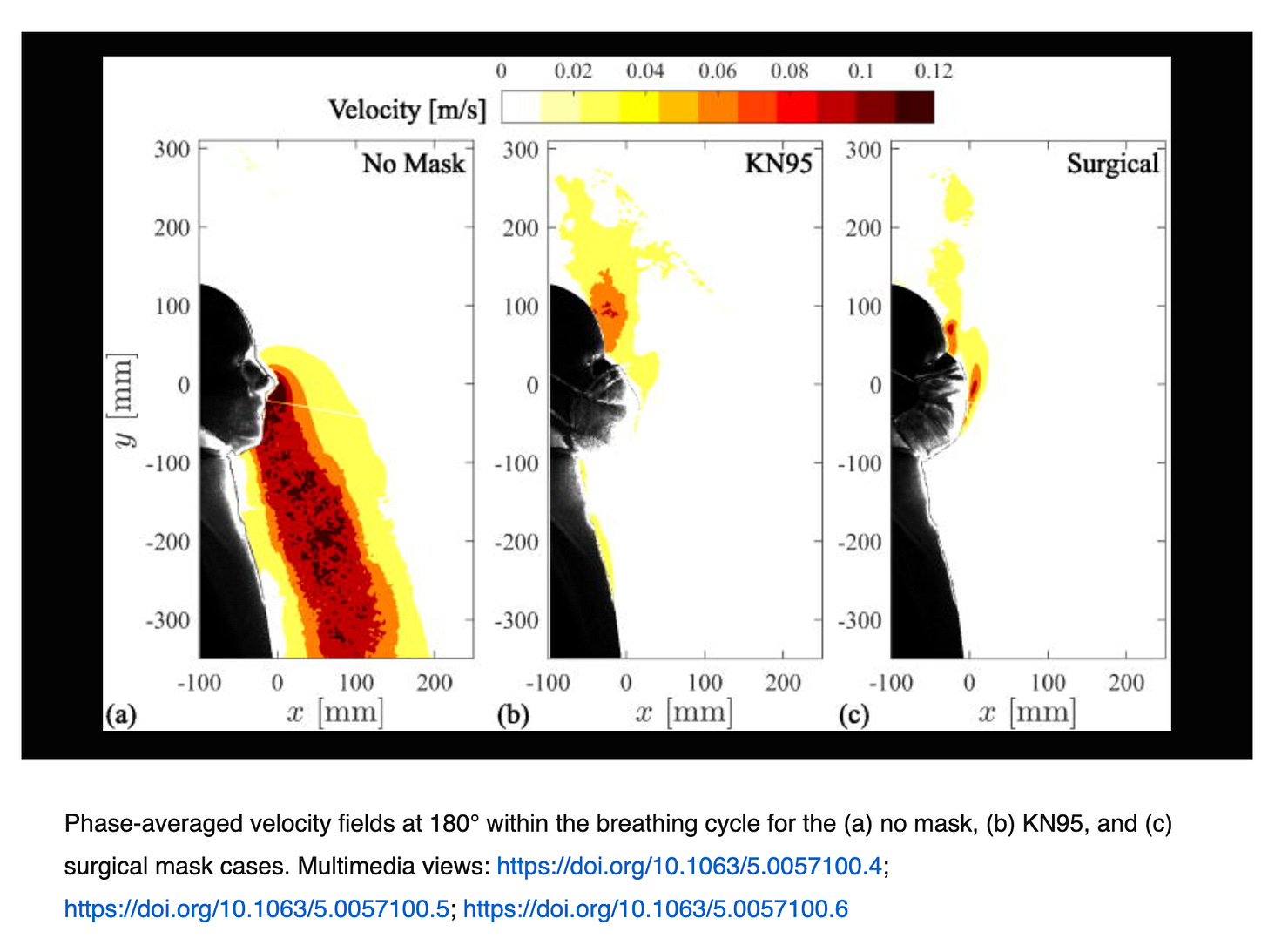
Figure 6(a) in the excerpt below is the most important. The graph maps the portion of particles that escape from the mask by mask type, and without mask (the black line). What it shows is that surgical masks do reduce the number of particles emitted at all sizes, but not by much. KN95s are a bit better, and N95s are quite a bit better. But it is important to look at 6(b) to put this into perspective. Many of the claims about mask efficacy have relied on the material’s ability to filter without accounting for gaps. That is what is shown in 6(b). In that figure, all of the masks are quite efficient at removing particles—as long as there is a rubber gasket or silicon caulking attaching them to your face, i.e. so long as there are no gaps at all. Figure 6(c) is, interesting. What figure 6(c) shows for each scenario is the proportion of particles of each size. What it specifically shows is that for each mask type, while the mask may filter out more or less particles, they each filter exactly the same percent of particles of all size—that is, the size of the particle is not important for filtration. This is at odds with other findings, and we will address potential causes for this discrepancy at the end of this discussion. 6(d) on the right is the same, but for the particles that escaped from the mask materials without gaps. Here there is a difference, and what it shows is that when forced through the filter of the mask (versus going around through the gaps), there are significant difference both by particle size, and by mask type. What it shows is that N95s have the highest portion (not absolute number) of particles escaping in the <0.3 micron range, and then markedly lower above that threshold. This is actually exactly what ought to happen. N95s are rated to filter out 95% of particles larger than 0.3 microns when properly fit-tested. The fact that 6(c) shows no difference in the distribution of particles shows that the lack of filtration is a function of leakage, and all the particles are basically following the airflows, being filtered at the same rate (again, this is actually at odds with other research, so we will return to this at the end of the paper).
Excerpt 6

Before we move on to the second portion of the study, which is more qualitative, let’s try and tease out what these numbers mean for the utility of masks in decreasing the transmission of viral respiratory disease from person-to-person
Since we now know that COVID is predominantly spread by very small and extremely numerous aerosols roughly the same size as cigarette smoke, like cigarette smoke it is virtually instantly all around you. There is a sort of “common sense” logic that says, “well, even if there are only 20% fewer particles, or even 2-3% fewer particles, that means I’m that much less likely to get sick,” but that’s not how it works. This is because the minimum infective dose of COVID, that is, the minimum number of viral particles you need to be exposed to in order to get sick, is very small. There are now a whole host of studies that suggest that the minimum infective dose for COVID is between 100 and 1000 virions, with a recent review suggesting that the more likely number was around 100 virions as the minimum infective dose.
Now let’s compare this to the number of virions or virus particles that an infected person exhales. 10 million per hour—that was the average number exhaled and captured in a recent study—the same study showed that some patients exhaled literally billions per hour. Based on a minimum infective dose of 100-1000 virions referenced above, this would mean that the exhalations from a single sick person would be capable of getting between 10,000 and 100,000 people sick (obviously not physically possible)—in just one hour. Nor is this an outlier. Another study identified that SARS-CoV2 positive patients exhaled between ~15,000 and 450,000 infective doses per hour—the upper end being enough infectious virus to get 126 people sick every second.
What does that mean for the efficacy of masks in preventing disease? Nothing good. Our study shows that, of the aerosols that are most likely to carry infectious virus, those from 0.2 - 1 micron, masks stop from ~20% (surgical masks) to ~62%—80% on the high end (N95s). Let’s say you’re in a large room (say 20’ x 20’) with an infected person for an hour. Based on the low-end number cited above, that would mean there are roughly 15,000 “doses” (~100 virions) invisibly floating around you. Would a 20% reduction to 12,000 (the equivalent of wearing a surgical mask) make you significantly less likely to make contact with these invisible things? Of course not—particularly as the aerosols carrying the individual virions that make up that “dose” are even more diffuse. What if that number were reduced by 80%, and there were only 3,000 doses invisibly floating through the air? Would you feel sanguine in your about your ability to “dodge” all of those 3000 invisible things? Put another way, if there were 5 people smoking across the room, would you be less likely to smell the virus if there were only 4 people smoking? What if there were only one? The answer of course, “no”.
Another compounding factor is that different people exhale more or less of these infectious aerosols. In the study above, there is more than a 30-fold difference between the highest emitter and the lowest. Meaning, you might reduce the emissions by 80%, but an 80% reduction for the person on the high end would still result in that person exhaling 90,000 infectious doses per hour—6 times more than the un-masked person on the low-end. This is, unfortunately a theme throughout much of the COVID-19 research—a very small percentage of people are responsible for producing the vast majority of the infectious aerosols. This study found that 3.5% of the participants exhaled more than 50% of the aerosols. People who are sick with COVID-19 exhale orders of magnitude of aerosols, and especially those in the smallest, most numerous, and most infectious range, <0.3 microns. Older and sicker people also generally have higher aerosol exhalation rates. What’s worse, is that it has repeatedly been found for both COVID and flu, that when people are infected with viruses carried by these smallest—and most numerous—aerosols, as opposed to via droplets/saliva, they get sicker, despite lower counts of viral copies/infective doses than saliva. Then there is the other challenge that these aerosols stay afloat basically indefinitely, and remain infectious for at least three hours.
What does that mean for how quickly you can get infected, being in a room with an infected person, or in a room an infected person has recently occupied? Literally minutes, according to this study (which is a modeling study, and hence not super reliable, but nonetheless).
A friend of mine, Megan Mansell, has done yeoman’s work on this, and the reading is very much worth your while.
The disease modality we wrongly apply to respiratory viruses is one of exposure—the more exposure the greater the likelihood of your contracting the disease, like lung cancer from smoking, or cirrhosis from drinking. Given the extremely small minimum infective dose, and the extremely large number of infective doses exhaled by people ill with respiratory viruses, we would be better served to think of exposure as roughly binary, akin to our ability to smell something like smoke.
This came home to me very powerfully when I was doing some “smoking videos” in 2021 to visually demonstrate the ineffectiveness of masks at capturing small aerosols of the size that have been shown to carry the bulk of infectious virus. I did these “tests” upstairs in my bathroom with the windows open, and the doors closed. Yet, the minute my kids walked in the door from school (probably 150 linear feet away), they smelled it, and yelled up “Mom, you promised you wouldn’t do any more smoking videos!” (They were worried I would get insta-cancer).
Video 1
Understanding this, let’s revisit the pee analogy that was so widely deployed at the beginning of COVID.
While this is compelling, it is completely inaccurate for something spread via sub-micron aerosols. A more accurate analogy to the effectiveness of masks would be peeing in a swimming pool. Using masks as a means of stopping transmission are akin to having a rule that you can pee in the pool, as long as you’re wearing a swimming suit. Will some of the urine stay on the suit? Sure. But not a lot, and the longer you’re moving around in the pool the less there will be on/in it.
Now let’s turn to the more qualitative aspects of the study. The study also demonstrated the flow of particles both with and without the various masks. As you can see in excerpt 9 below, the masks redirect the air, up and out, with varying degrees of focus, depending on the mask. The 2021 study completed by the same group used the nose as the point of exhalation instead, and in that case, as shown in excerpt 10, you can see that the exhalation is directed down.
Excerpt 9
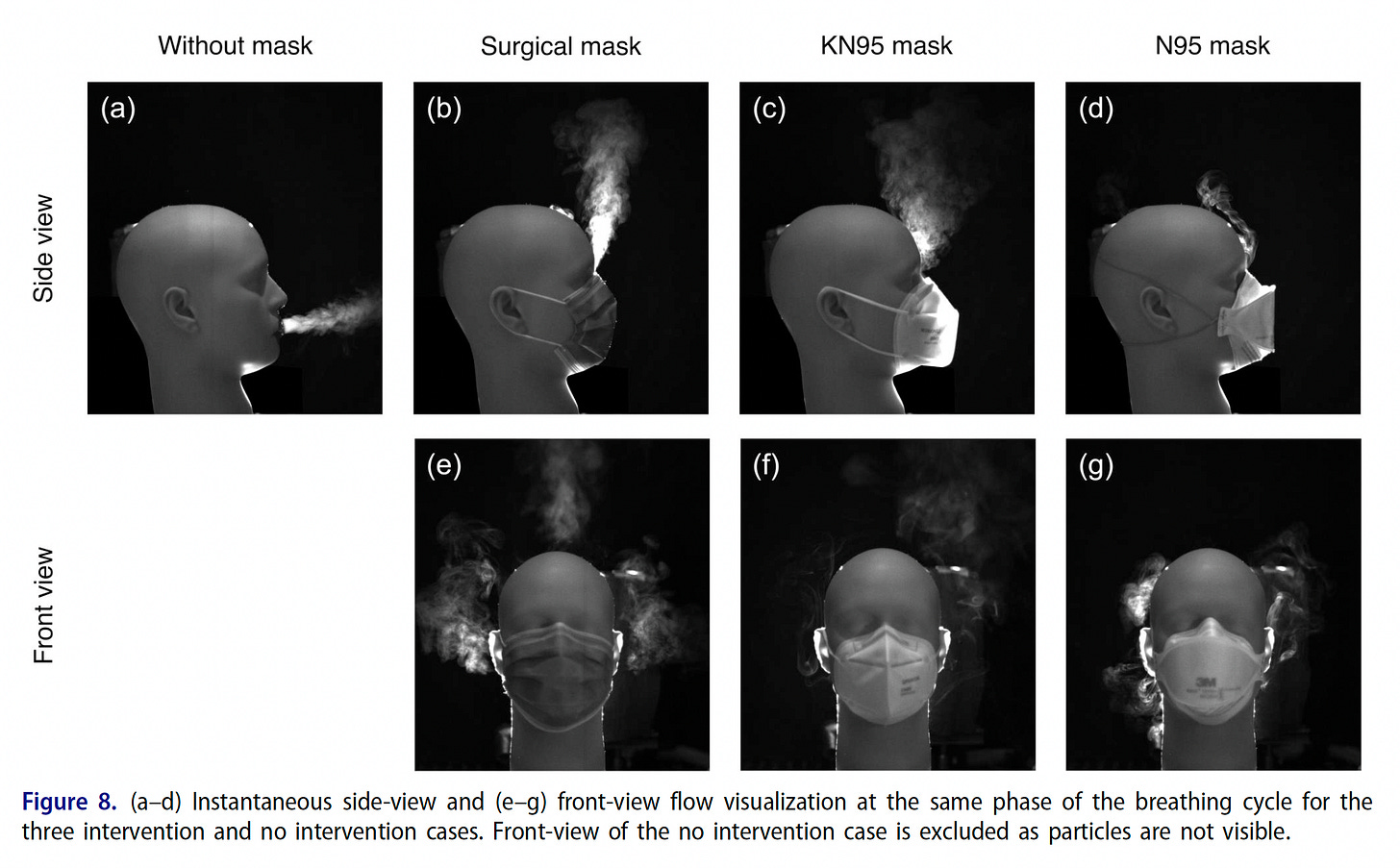
Excerpt 10
This concept of air redirection was used for some of the most base and pathetic mask propaganda, shown in Video 2 below. On the right, Bill Nye the “Science” guy, shows how effective masks are at stopping him from blowing out the candle. On the left though, you can see that if you simply move the flame over the mask, the flame is just as easy to extinguish as if there were no mask—demonstrating that the air has solely been redirected. (You’ll have to click through to Twitter to watch the video—which I strongly recommend.)
Video 2
So how can we use this information? First of all, it is important to remember this study does not tell us the ability of any mask to stop the transmission of respiratory viruses to another person. What it does tell us, is the relative efficacy with which masks of various types filter the sub-micron particles most likely to carry COVID-19, and it shows us the trajectory of those aerosols (as exhaled by a mannequin). Using that information, we can extrapolate, based on the minimum infective dose of COVID-19, and the number of virus particles/virions/RNA copies exhaled per hour or per breath, how effective each mask type is in impacting transmission of respiratory viruses such as COVID-19. Based on these calculations, the answer would seem to be virtually non-existent (which is in accordance with all of the extant systemic reviews of the extant randomized trials, as referenced at the beginning of this piece). It is also borne out repeatedly in the “natural experiments” conducted during the COVID period (which are only relevant if they are geographically virtually identical, as the example below is).
Figure 2
But let us instead focus on the applicability of this use case to the situations where we are currently most likely to encounter masks: healthcare settings. I recently had the misfortune of going to a doctor and being asked to put on a mask (yes, in Texas). Let us try and evaluate the likely efficacy of that action, which I was told was necessary to protect the providers in the room (who were not wearing masks). First of all, I was given a KN95, which the authors noted in their 2021 study was, if it had a 3 millimeter gap, only 5 percent effective at stopping aerosols (and which, again, does not take into effect the very low minimum invective dose of COVID, and the very high number of extremely contagious virus-carrying aerosols exhaled during breathing). Next, let’s think about the actual visit. When I arrived, I was offered a water, which of course allowed me to take my mask down to drink. Then, I got a throat swab, during which I naturally had to lower my mask. But let’s focus instead, just on the time that I had my mask on. During that time, my KN95, which absolutely had a 3 millimeter gap, effectively directed all of the aerosols I exhaled straight into the nostrils of my practitioners (who were not wearing masks, because masks were solely used for source control in this practice). Had I not had a mask, those same aerosols would largely have been directed down. Probably wouldn’t have made much difference, as they are so numerous, and basically aloft indefinitely, but even so. What is interesting about his scenario, is even in a scenario with significant ventilation, the use of the mask whilst being attended by someone hovering over you, almost certainly would exacerbate that person’s risk of contracting COVID—or any other respiratory aerosol.
Another interesting potential example, is air travel. Here, too, the masks and their redirection of aerosols up and to the sides would be certain to put other passengers at greater risk, not less. While the natural trajectory of our breathing is out and down, and hence most likely to be caught up in the circulating currents of the plane’s air filtration system, which also point down, masks force the aerosols up, which would create a turbulence, almost certainly resulting in broader distribution throughout the plan—and certainly into the nostrils of the flight attendant, if they happened to be nearby. We can also see, that masks force aerosols out the sides—directly into the faces of adjacent passengers. Given the laminar air flows, it is hard to envision a scenario where masks do anything but increase the likely exposure of others, particularly in close quarters.
Figure 3

From my perspective, this new data, coupled with recent studies on minimum infective dose, and others quantifying the amount of virus—and especially infectious virus—carried in every liter of exhaled air, argues powerfully that masks as a means of halting transmission are ineffective at best, and in some cases, such as healthcare settings and planes, where people “hover” over or near others, they may in fact increase the risk of transmission to people in their immediate vicinity.
But what about protection? If the healthcare workers in my doctor’s office were primarily concerned with reducing their own risk of infection, and if my wearing a mask does not protect them, should they instead wear masks? The answer is, I think, “It depends.” N95s are rated for protection for particles greater than 0.3 microns, they are not rated to stop release of such particles. Physically, there is a significant difference between protecting against things coming in and stopping things going out—when you inhale, the fit of the mask becomes tighter, due to the vacuum created, thus increasing the likelihood of filtration. When you exhale the opposite happens.
However, protection depends on compliance. When considering the impact of "breaks,” a randomized controlled trial from 2013, found that N95’s did reduce the risk of disease, but only if worn continuously, without breaks— the protection effects disappear once breaks are introduced. This squares well with the data above, which would suggest that “mask breaks” of any kind are akin to punching a giant hole in the bottom of your boat.
There are cases, and people where real protection is needed, but it is important that we not tell them they are protected when they are not. Such misinformation provides a fall sense of security, which could lead to engagement in riskier behaviors, which, depending upon the person’s risk profile, or the hazard profile, could put them in real danger. An honest statement about the level of protection provided would instead lead to more cautious behaviors, or seeking out more effective forms of protection when needed (e.g. when people are working with truly dangerous pathogens, you don’t see them wearing masks, you see them virtually in a bubble).
So where does that leave us? What have we learned about the ability of masks to prevent the transmission of respiratory disease? We now have a mechanistic study that helps to explain, in conjunction with a host of other recent and older research, why the use of masks in randomized controlled trials does not prove effective at stopping transmission of respiratory disease, even though a whole host of mechanistic studies and poorly designed observational studies suggest they should.
Where do we go from here? One could argue that we need yet another randomized controlled trial, but we have a large number of these, as well as multiple systemic reviews of these, all demonstrating no effect. Indeed, there has been significant concern that surgical masks are ineffective even in their main purpose, which is preventing the spread of bacteria, and reducing infections of patients during surgery—which involve much larger particle sizes. Why would we think they would show greater efficacy in stopping respiratory aerosols that are orders of magnitude smaller, and which behave far more like gases than liquids?
Excerpt 11
Thus, it hardly seems necessary to do yet another RCT. Rather, is seems that a better approach would be to acknowledge that the protection which we perceive masks offer is a false perception, and in places where exposure truly needs to be minimized, provide people with real protection. As it things stand now, we are giving people seatbelts that aren’t attached to the car. But only after an accident will they realize the lack of safety they were provided.
The last thing we need to address are some discrepancies in this research with prior research. The authors of the current study being discussed, produced another similar study a few years back, in 2021. That study had a larger particle size, with the average particle size being 1 micron vs. 0.5 micron in this most recent study. Yet with average particles more than twice the size, the prior study showed (excerpt 12 below) substantially lower mask filtration efficiency, with cloth masks and surgical masks demonstrating ~10% (half the current study), and KN95s with a 3mm gap showing ~5% filtration efficiency.
Excerpt 12

Excerpt 13

Another study, which was referenced in the current study examined filtration efficiency in face masks for particles as small as 0.34 microns. The filtration efficiency, shown in excerpt 14 below is closer to what was seen in the 2021 paper, at roughly 10% for the more physiologically representative test (15 L/min breathing). But notable is a clear and consistent decline in the filtration efficiency as particle size goes down. This result conflicts with the 2025 study we are discussing here.
Excerpt 14

The question is, what accounts for the difference in the filtration efficiencies? Why does a study looking at smaller particles show greater filtration efficiency? Why is there a decreasing filtration efficiency tightly tied with size in other studies, but not in this one?
There are several possible explanations—most likely to do with experimental set-up.
Excerpt 15

There are several differences between the two set-ups. First, is the size of the rooms. In the 2021 study, the room was a much larger room, 7.8 m x 5.7 m x 2.7 meter, or appx. 22’ x 17’ x 8’, and the measurement was taken at 2 meters from the location of the mannequin. The study published in 2025 [“the current study,” hence forth], used a much smaller space, 0.64 m x 0.64 m x 0.91 m. Thus, the 2021 study was evaluating the concentrations in a room of nearly 2000 cubic feet, or ~85,000 liters, the the current 2025 study measured total concentration in a space of just 18 cubic feet, ~500 liters, and approximately 166 times smaller. Both studies were conducted in unventilated spaces, which would have had no air currents except those created by the breathing piston. In the smaller space of the 2025 study, the aerosols would necessarily have stayed very close to the mask, possibly resulting in re-filtration by the masks. In one of the referenced articles, it was explicitly noted that rebreathing artificially increased filtration, particularly when the volumes are high. While at 7.5 liters/minute, the exhalation and inhalation volumes in this current study are not high, relative to the size of the chamber they are—in fact, this is equivalent to approximately 1.5% of the chamber volume. This means that the entire contents of the chamber could be re-breathed in just over an hour—and the experimental set up lasted two hours. Further, as the only movement in this limited space, the ebb and flow of breathing may well have kept the exhaled aerosols right by the masks, ebbing and flowing like waves on a shore, and constantly being refiltered by the masks. This would seem to be much less likely in the 2021 experimental set-up, first, because the tidal breathing volume represented 0.009% of the room volume, and second, also possibly because the sampling was taken at a location two meters away from the mannequin. Obviously, in a real-world situation, a person would exhale, and whatever particles were nearby him or her would not be re-filtered, but would be largely be taken away on whatever air currents happened to be in the room—indeed the authors demonstrated in their 2021 study that when even modest ventilation was introduced, particle concentrations dropped by close to 2/3rds. These, and perhaps other differences may explain the differences in the filtration efficiencies, and the non-size-based filtration seen in the current study (please add your ideas in the comments, if you have others).
Disclosures: This study was funded by Restore Childhood, an organization to which I have provided funding, and of which I used to be an un-paid board member.







This from Emily is a lot to go through. One of my base attitudes about mask ineffectiveness is, Why is it that in the early 2020s an unusually high number of people globally died from respiratory illnesses, just when wearing a mask became widespread and mandated in most countries?
If masks are effective, wearing them should have decreased virus transmission enough to cause a reduction in covid deaths. Instead, deaths went much higher after wearing them was mandated. When mask wearing became unusual, covid deaths decreased.
This is an absolute tour de force, thanks :)